Early Online (Volume - 9 | Issue - 1)
Gilbert’s Syndrome Revealed by Hepatotoxicity of Imatinib
Published on: 12th March, 2025
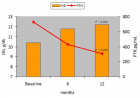
Gilbert’s Syndrome (GS) is a hereditary disease that can cause hyperbilirubinemia due to a mutation in the promoter of the UGT1A1 gene, which causes a decrease in uridine diphosphate glucuronyltransferase enzyme activity. Polymorphisms in the UGT1A1 gene are associated with induced hyperbilirubinemia by Tyrosine Kinase Inhibitors (TKI) in Chronic Myeloid Leukemia (CML). We report a case of patient who developed hepatotoxicity when treated on Imatinib and subsequently diagnosed with Gilbert’s syndrome. Eight months after initiating Imatinib, the patient developed conjunctival jaundice and signs of hepatotoxicity with increase in liver enzymes and hyperbilirubinemia with elevated level of unconjugated bilirubin. Gilbert’s syndrome was suspected in the presence of predominantly unconjugated hyperbilirubinemia and a prior history of transient episodes of jaundice. Genetic testing revealed homozygosity for the UGT1A1 TA7 (*28) polymorphism. Imatinib was stopped due to continuous increase of aminotransferases and hyperbilirubinemia and restarted after improvement of Liver Function Tests (LFTs) with a reduced dose of 200 mg/day but LFTs worsted again, and the patient was switched to Dasatinib 100 mg/day, without hepatic cytolysis and a mild persistent hyperbilirubinemia after a follow up of 20 months.Patients with an unexplained rise in serum bilirubin levels on Imatinib therapy should be screened for the genetic UGT1A1 polymorphisms.
The Synergistic Effect of Combined Linagliptin and Metformin Improves Hepatic Function in High-fat Diet/Streptozotocin-induced Diabetic Rats
Published on: 2nd June, 2025
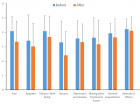
Background: Monotherapy for liver dysfunction in diabetes is less effective. This study investigated the effect of combined linagliptin and metformin therapy on liver function in diabetic rats. Methods and materials: Sixty-four mature male (200-300 g) Wistar rats were used. Streptozotocin (35 mg/kgb.wt) was repeatedly injected intraperitoneally to induce diabetes. The rats were grouped into eight groups (n = 8). Group I: control; Group II: control + 10 mg/kgb.wt linagliptin; Group III: control + 200 mg/kgb.wt metformin; Group IV; control + 10 mg/kgb.wt linagliptin + 200 mg/kgb.wt metformin; Group V: diabetic; Group VI: diabetic + 10 mg/kgb.wt linagliptin; Group VII: diabetic + 200 mg/kgb.wt metformin; Group VIII: diabetic + 10 mg/kgb.wt linagliptin + 200 mg/kgb.wt metformin. The animals were sacrificed on the last day of the experiment, blood and liver samples were collected for biochemical assay. Results: Insulin, blood glucose, glycated hemoglobin, total cholesterol, triglycerides, low-density lipoprotein cholesterol (LDL-cholesterol), liver function biomarkers, liver glucose metabolic enzymes, malondialdehyde and inflammatory markers increased (p < 0.05) significantly. High-density lipoprotein-cholesterol (HDL-cholesterol), liver antioxidant, glycogen, and glycogen synthase were reduced significantly in diabetic rats. Linagliptin and metformin administration single and combined reduced the insulin, blood glucose, glycated hemoglobin, total cholesterol, triglycerides, LDL-cholesterol, liver function biomarkers, liver glucose metabolic enzymes, malondialdehyde, and inflammatory markers, and increased the HDL-cholesterol, liver antioxidant, glycogen and glycogen synthase in diabetic rats.Conclusion: Linagliptin monotherapy alone efficiently controls hyperglycemia and remarkably improves liver functions. Combining linagliptin and metformin could be used as safe and effective therapy for liver dysfunction progression in diabetes.
A Rare Case of Cytomegalovirus Colitis Mimicking Colon Adenocarcinoma in an Immunocompetent Patient
Published on: 11th July, 2025
Cytomegalovirus (CMV) colitis is classically seen in immunocompromised individuals, such as those with HIV, organ transplants, or receiving immunosuppressive therapy. It is exceedingly rare in immunocompetent patients and can pose a diagnostic challenge, especially when it presents as a mass-like lesion mimicking colon cancer. We report a case of a 78-year-old immunocompetent male who presented with hematochezia and was found to have a bleeding cecal mass initially suspicious for adenocarcinoma. Subsequent histopathology revealed CMV colitis. This case emphasizes the importance of considering CMV colitis in the differential diagnosis of colonic masses, even in immunocompetent hosts.
Study of Platelet Parameters in the Assessment of Disease Severity in IBD: Ulcerative Colitis
Published on: 8th August, 2025
Background: Platelets are increasingly recognized as important inflammatory markers. This study explores the association between platelet indices and disease severity in ulcerative colitis (UC).Objective: To evaluate platelet parameters in patients with newly diagnosed UC and assess their correlation with disease severity indices.Methods: A cross-sectional observational study was conducted at IMS & SUM Hospital, Bhubaneswar, between October 2022 and September 2024. A total of 62 newly diagnosed UC patients aged over 18 years were included. Disease severity was evaluated using Truelove and Witts (TLW) criteria, Mayo Disease Activity Index (Mayo DAI), and Ulcerative Colitis Endoscopic Index of Severity (UCEIS). Platelet count, mean platelet volume (MPV), platelet distribution width (PDW), platelet mass index (PMI), and platelet large cell ratio (PLCR) were measured. Statistical analysis included Pearson correlation, ROC curves, and sensitivity/specificity assessment.Results: The majority of patients were male (81%) with a mean age of 28.2 years. A significant positive correlation was observed between platelet count and disease severity by UCEIS (r = 0.32, p = 0.015) and Mayo DAI (r = 0.35, p = 0.009). PMI showed strong correlations with UCEIS (r = 0.45, p = 0.001) and Mayo DAI (r = 0.48, p < 0.001). MPV was inversely correlated but showed weak significance. PLCR also showed significant correlations. ROC analysis revealed platelet count (AUC = 0.815) and PLCR (AUC = 0.729) as good predictors of disease severity.Conclusion: Platelet parameters, particularly PMI, PLCR, and platelet count, may serve as accessible, non-invasive biomarkers for assessing disease severity in UC. Further studies with larger cohorts are warranted.

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."