More Information
Submitted: September 20, 2021 | Approved: October 11, 2021 | Published: October 12, 2021
How to cite this article: Danish M, Khan SA, Samoon D, Majid Z, Hanif F, et al. Diffuse large B-cell Lymphoma mimicking as cholangiocarcinoma in a young male presenting with obstructive jaundice. Ann Clin Gastroenterol Hepatol. 2021; 5: 039-040.
DOI: 10.29328/journal.acgh.1001031
Copyright License: © 2021 Danish M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Diffuse large B-cell Lymphoma mimicking as cholangiocarcinoma in a young male presenting with obstructive jaundice
Muhammad Danish1*, Shoaib Ahmed Khan1, Dilnawaz Samoon1, Zain Majid2, Farina Hanif3, Abbas Ali Tassneem3 and Nasir Hasan Luck4
1Post Graduate Trainee, Pakistan
2Consultant, Pakistan
3Associate Professor, Pakistan
4Professor, Pakistan
*Address for Correspondence: Muhammad Danish, Post Graduate Trainee, Pakistan, Email: [email protected]
The involvement of bile duct in lymphoma is considered to be very rare and is usually a sequela of a disseminated disease [1]. In contrast to secondary involvement, primary non-Hodgkin’s lymphoma arising from the bile duct is extremely rare and presents with obstructive jaundice [2,3]. Non-Hodgkin’s lymphoma (NHL) accounts for 1% - 2% of all cases of malignant biliary obstruction [4]. Hepatobiliary involvement by malignant lymphoma is usually a secondary manifestation of systemic lymphoma. The first case of Non-Hodgkin lymphoma arising from bile duct was described by Nguyen in 1982 [5]. Most common extra nodal involvement of NHL is abdomen. Although, involvement of the stomach, pancreas or common bile duct is not common [6]. We present to you a case of 31year old male who presented to us with obstructive jaundice and was later diagnosed as Diffuse Large B-Cell lymphoma.
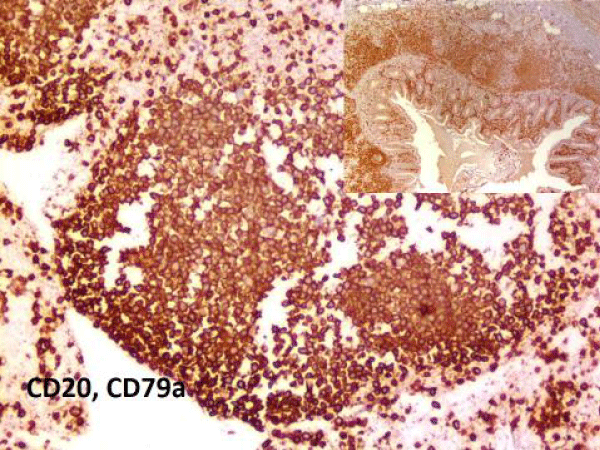
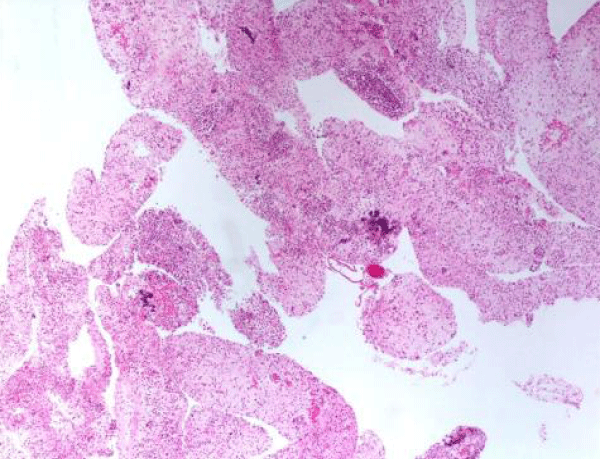
31 year old male, farmer, presented to us with 2 months’ history of epigastric pain which was localized, no radiating and not associated with postural change and meal intake. He does complain of jaundice which was gradual in onset and associated with itching, darkening of urine and clay colored stool. On examination, he had BMI of 16 and was icteric while rest of the general physical examination and systemic examination was unremarkable. His laboratory investigations revealed Hb of 13.2, TLC of 6.4, Platelets of 427, Total Bilirubin of 24.7 with direct bilirubin of 12.7, Alkaline phosphatase of 333, ALT of 98 and AST of 163. ESR was 78. His CT scan showed irregular solid hypo dense lesion with exophytic component in segment III and IV b of liver showing delayed enhancement measuring 6.9 x 5.4 cm and was indenting left branch of portal vein and infiltrating hepatic capsule and the suspicion was likely of cholangiocarcinoma with loco regional lymphadenopathy with intrahepatic ductal dilatation. So in order to decompress the biliary system, he first underwent ERCP which revealed tight stricture at mid CBD level with proximal intrahepatic ductal dilatation and stenting was done. Then he underwent Endoscopic Ultrasound guided left lobe of liver Nodal mass biopsy which revealed lymphoproliferative disorder on the basis of morphological features and IHC profile. To further confirm it, he underwent liver lesion core needle biopsy which showed Diffuse Large B cell lymphoma. On PET scan it was further staged as Ann Arbor Stage I. He received 4 cycles of R-CHOP chemotherapy and currently LFTs are normal and Repeat CT scan post treatment confirmed no evidence of any residual disease and he was made stent free (Images 1,2).
Image 1: Shows liver tissue which is diffusely positivity for CD 20 and CD 79a (IHC marker).
Image 2: Shows the liver tissue on which hematoxylin and eosin stain (H&E) is applied.
Non-Hodgkin lymphoma (NHL) accounts for 1% - 2% of all cases of malignant biliary obstruction [7]. Diffuse large B cell lymphoma (DLBCL) is the most common lymphoid neoplasm and the most common histologic subtype of NHL, accounting for approximately 25% of all cases [7,8]. In DLBCL, most of patients are diagnosed in the seventh or eighth decade of life with male: female ratio of 2:1 [8,9]. How ever in our case the DLBCL appears in young age which is unique in terms of age presentation. The DLBCL typically presents with rapid nodal enlargement in the neck or abdomen, and systemic” symptoms are observed in 30% of patients [10]. There have been many recent reports of success with EUS-FNB for a definitive tissue diagnosis [11]. In our case, the EUS-FNB was tried, but tumor could not be pointed out clearly. There are a number of reasons for Jaundice in lymphoma patients. It can either be secondary due to direct hepatic involvement [12], or can occur as a consequence of extrahepatic bile duct obstruction due to enlarged lymph nodes [13]. Lastly can be due to intrahepatic cholestasis, toxic hepatitis due to drug treatment, or tumor related hemolysis [14]. It is difficult to diagnose primary lymphoma of the CBD on the basis of CT scan, MRI, and cholangiography results, because in most cases, these clinical and radiological findings resemble those of bile duct carcinoma. Yoon, et al. reported that radiologists should raise the contingency of primary biliary tree lymphoma when cholangiography shows smooth, mild luminal narrowing of the extrahepatic biliary channels without mucosal irregularities, in spite of the diffuse thickening of the ductal wall on CT/MRI [15].
The treatment management of resectable hilar cholangiocarcinoma and lymphomas could differ greatly and that radical resection of bile duct malignancy includes the possibility of high morbidity, it is very important for radiologists to suggest the possibility of primary biliary lymphoma when cholangiography shows smooth, mild, luminal narrowing of the extrahepatic bile duct without mucosal irregularity, despite diffuse thickening of the ductal wall on CT/MR images.
In conclusion, despite the sparsity of published medical reports, primary lymphoma of the extrahepatic bile duct should be considered in the differential diagnosis when a patient with obstructive jaundice presents with discrepant imaging findings on CT or MRI and ERCP. Multiple, deep biopsies from the biliary segment of the suspected lesion are mandatory in order to establish a definitive diagnosis before further treatment.
- Kang CS, Lee YS, Kim SM, Kim BK. Primary low grade B cell lymphoma of mucosa associated lymphoid tissue type of the common bile duct. J Gastroenterol Hepatol. 2001; 16: 949-951. PubMed: https://pubmed.ncbi.nlm.nih.gov/11555119/
- Joo YE, Park CH, Lee WS, Kim HS, Choi SK, et al. Primary non-Hodgkin’s lymphoma of the common bile duct presenting as obstructive jaundice. J Gastroenterol. 2004; 39: 692-696. PubMed: https://pubmed.ncbi.nlm.nih.gov/15293142/
- Eliason SC, Grosso LE. Primary biliary malignant lymphoma clinically mimicking cholangiocarcinoma: a case report and review of the literature. Ann Diagn Pathol 2001; 5: 25-33. PubMed: https://pubmed.ncbi.nlm.nih.gov/11172204/
- Lokich JJ, Kane RA, Harrison DA, McDermott WV. Biliary tract obstruction secondary to cancer: management guidelines and selected literature review. J Clin Oncol. 1987; 5: 969-981. PubMed: https://pubmed.ncbi.nlm.nih.gov/3295131/
- Nguyen GK. Primary extranodal non-Hodgkin’s lymphoma of the extrahepatic bile ducts. Report of a case. Cancer. 1982;50: 2218-2222. PubMed: https://pubmed.ncbi.nlm.nih.gov/7127262/
- Yang T, Pan J, Zou Y. Obstructive Jaundice caused by Non-Hodgkin Lymphoma in common bile duct. J Pediatr. 2015; 167: 1168-1168. PubMed: https://pubmed.ncbi.nlm.nih.gov/26340876/
- Swerdlow SH, Campo E, Harris NL, et al. World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon: IARC Press; 2008
- Kallab A. Diffuse large B cell lymphoma. Medscape. 2013
- Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, et al. Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood. 2006; 107: 265-276. PubMed: https://pubmed.ncbi.nlm.nih.gov/16150940/
- Armitage JO, Weisenburger DD. New approach to classifying non-Hodgkin’s lymphomas: clinical features of the major histologic subtypes. Non-Hodgkin’s Lymphoma Classification Project. J Clin Oncol. 1998; 16: 2780-2795. PubMed: https://pubmed.ncbi.nlm.nih.gov/9704731/
- Coiffier B. State-of-the-art therapeutics: diffuse large B cell lymphoma. J Clin Oncol. 2005; 23: 6387–6393. PubMed: https://pubmed.ncbi.nlm.nih.gov/16155024/
- Birrer MJ, Young RC. Differential diagnosis of jaundicein lymphoma patients. Semin Liver Dis. 1987; 7: 269–277. PubMed: https://pubmed.ncbi.nlm.nih.gov/3317863/
- Feller E, Schiff Man FJ. Extrahepatic biliary obstruction by lymphoma. Arch Surg. 1990; 125: 1507–1509. PubMed: https://pubmed.ncbi.nlm.nih.gov/2241566/
- Rosenberg SA, Diamond HD, Jaslowitz B, Craver LD. Lymph sarcoma: a review of 1269 cases. Medicine. 1961; 40: 31–84. PubMed: https://pubmed.ncbi.nlm.nih.gov/13743408/
- Yoon MA, Lee JM, Kim SH, Lee JY, Han JK, et al. Primary biliary lymphoma mimicking cholangiocarcinoma: a characteristic feature of discrepant CT and direct cholangiography findings. J Korean Med Sci. 2009; 24: 956–959. PubMed: https://pubmed.ncbi.nlm.nih.gov/19794999/